TYLER, Texas — The U.S. Food and Drug Administration (FDA) has added a new warning for consumers stating the single-dose Johnson & Johnson COVID-19 vaccine can lead to an increased risk of a rare condition known as Guillain-Barré syndrome (GBS).
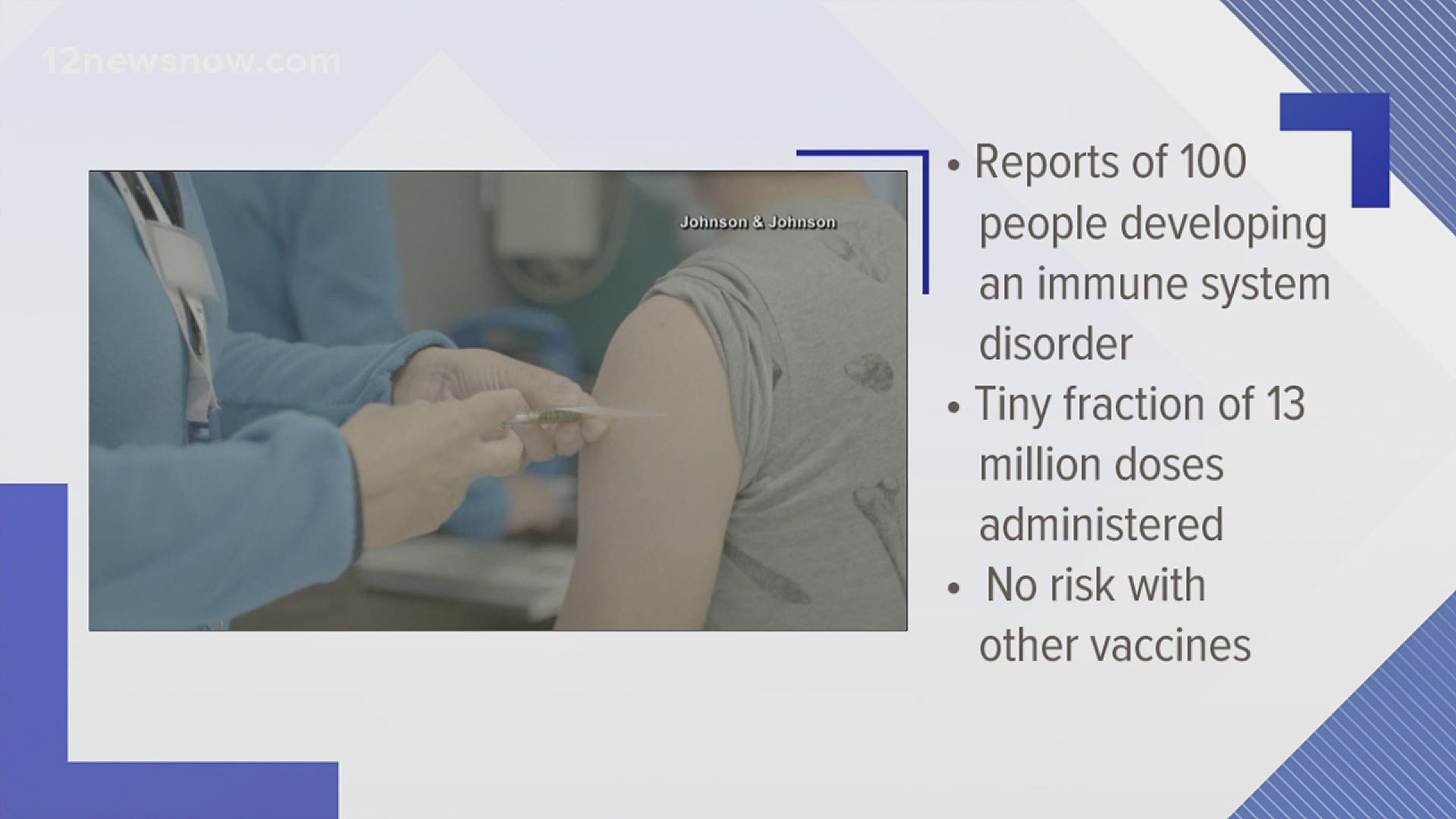
The action comes after the FDA and the Centers for Disease Control and Prevention (CDC) reviewed reports of about 100 people developing the syndrome after receiving the shot. Almost all of them required hospitalization and one person died, the FDA said.
Johnson & Johnson says most GBS cases occurred within 42 days after vaccination.
"While the chance of having this occur is very low, Johnson & Johnson has updated its COVID-19 Vaccine Factsheet to include important information about these rare cases and on the signs and symptoms of Guillain-Barré syndrome," the company said in a statement. "Updates with this new information will be implemented in other regions of the world according to local regulatory procedures"
So, what is Guillain-Barré syndrome?
According to the National Institute of Health (NIH), GBS is a rare neurological disorder in which the body's immune system mistakenly attacks part of its peripheral nervous system — the network of nerves located outside of the brain and spinal cord. GBS can range from a very mild case with brief weakness to nearly devastating paralysis, leaving the person unable to breathe independently. The NIH says, fortunately, most people eventually recover from even the most severe cases of GBS. After recovery, some people will continue to have some degree of weakness.
Guillain-Barré syndrome can affect anyone, according to the NIH. It can strike at any age (although it is more frequent in adults and older people) and both sexes are equally prone to the disorder. GBS is estimated to affect about one person in 100,000 each year.
What causes Guillain-Barré syndrome?
According to the NIH, the exact cause of GBS is unknown. Researchers don’t know why it strikes some people and not others. It is not contagious or inherited.
What they do know is that the affected person's immune system begins to attack the body itself. It is thought that, at least in some cases, this immune attack is initiated to fight an infection and that some chemicals on infecting bacteria and viruses resemble those on nerve cells, which, in turn, also become targets of attack. Since the body’s own immune system does the damage, GBS is called an autoimmune disease (“auto” meaning “self”). Normally the immune system uses antibodies (molecules produced in an immune response) and special white blood cells to protect us by attacking infecting microorganisms (bacteria and viruses). In GBS, however, the immune system mistakenly attacks the healthy nerves, the NIH says.
Most cases usually start a few days or weeks following a respiratory or gastrointestinal viral infection. Occasionally surgery will trigger the syndrome. In rare cases vaccinations may increase the risk of GBS.
What causes Guillain-Barré syndrome?
According to the NIH, unexplained sensations often occur first, such as tingling in the feet or hands, or even pain (especially in children), often starting in the legs or back. Children will also show symptoms with difficulty walking and may refuse to walk. These sensations tend to disappear before the major, longer-term symptoms appear. The NIH says weakness on both sides of the body is the major symptom that prompts most people to seek medical attention. The weakness may first appear as difficulty climbing stairs or with walking. Symptoms often affect the arms, breathing muscles, and even the face, reflecting more widespread nerve damage. Occasionally symptoms start in the upper body and move down to the legs and feet.
Most people reach the greatest stage of weakness within the first two weeks after symptoms appear; by the third week 90% of affected individuals are at their weakest, the NIH says.
In addition to muscle weakness, symptoms may include:
- Difficulty with eye muscles and vision
- Difficulty swallowing, speaking, or chewing
- Pricking or pins and needles sensations in the hands and feet
- Pain that can be severe, particularly at night
- Coordination problems and unsteadiness
- Abnormal heart beat/rate or blood pressure
- Problems with digestion and/or bladder control.
The NIH says these symptoms can increase in intensity over a period of hours, days, or weeks until certain muscles cannot be used at all and, when severe, the person is almost totally paralyzed. In these cases, the disorder is life-threatening — potentially interfering with breathing and, at times, with blood pressure or heart rate.
How is Guillain-Barré syndrome diagnosed?
According to the NIH, the initial signs and symptoms of GBS are varied and there are several disorders with similar symptoms. Therefore, doctors may find it difficult to diagnose GBS in its earliest stages.
The NIH says doctors will note whether the symptoms appear on both sides of the body (the typical finding in GBS) and the speed with which the symptoms appear (in other disorders, muscle weakness may progress over months rather than days or weeks). In GBS, deep tendon reflexes in the legs, such as knee jerks, are usually lost. Reflexes may also be absent in the arms. Because the signals traveling along the nerve are slow, a nerve conduction velocity test (NCV, which measures the nerve’s ability to send a signal) can provide clues to aid the diagnosis. There is a change in the cerebrospinal fluid that bathes the spinal cord and brain in people with GBS. According to the NIH, researchers have found the fluid contains more protein than usual but very few immune cells (measured by white blood cells). Therefore, a physician may decide to perform a spinal tap or lumbar puncture to obtain a sample of spinal fluid to analyze. In this procedure, a needle is inserted into the person’s lower back and a small amount of cerebrospinal fluid is withdrawn from the spinal cord. This procedure is usually safe, with rare complications.
Key diagnostic findings include:
- Recent onset, within days to at most four weeks of symmetric weakness, usually starting in the legs
- Abnormal sensations such as pain, numbness, and tingling in the feet that accompany or even occur before weakness
- Absent or diminished deep tendon reflexes in weak limbs
- Elevated cerebrospinal fluid protein without elevated cell count. This may take up to 10 days from onset of symptoms to develop.
- Abnormal nerve conduction velocity findings, such as slow signal conduction
- Sometimes, a recent viral infection or diarrhea.
How is Guillain-Barré syndrome treated?
According to the NIH, there is no known cure for GBS. However, some therapies can lessen the severity of the illness and shorten recovery time. There are also several ways to treat the complications of the disease.
Because of possible complications of muscle weakness, problems that can affect any paralyzed person (such as pneumonia or bed sores) and the need for sophisticated medical equipment, individuals with GuBS are usually admitted and treated in a hospital’s intensive care unit.
Acute care
The NIH says there are currently two treatments commonly used to interrupt immune-related nerve damage. One is plasma exchange (PE, also called plasmapheresis); the other is high-dose immunoglobulin therapy (IVIg). Both treatments are equally effective if started within two weeks of onset of GBS symptoms, but immunoglobulin is easier to administer. Using both treatments in the same person has no proven benefit.
In the process of plasma exchange, a plastic tube called a catheter is inserted into the person’s veins, through which some blood is removed. The blood cells from the liquid part of the blood (plasma) are extracted and returned to the person. This technique seems to reduce the severity and duration of the GBS episode. Plasma contains antibodies and PE removes some plasma; PE may work by removing the bad antibodies that have been damaging the nerves.
Immunoglobulins are proteins that the immune system naturally makes to attack infecting organisms. IVIg therapy involves intravenous injections of these immunoglobulins. The immunoglobulins are developed from a pool of thousands of normal donors. When IVIg is given to people with GBS, the result can be a lessening of the immune attack on the nervous system. The IVIg can also shorten recovery time. Investigators believe this treatment also lowers the levels or effectiveness of antibodies that attack the nerves by both “diluting” them with non-specific antibodies and providing antibodies that bind to the harmful antibodies and take them out of commission.
The NIH says anti-inflammatory steroid hormones called corticosteroids have also been tried to reduce the severity of GBS. However, controlled clinical trials have demonstrated that this treatment is not effective.
According to the NIH, supportive care is very important to address the many complications of paralysis as the body recovers and damaged nerves begin to heal. Respiratory failure can occur in GBS, so close monitoring of a person’s breathing should be instituted initially. Sometimes a mechanical ventilator is used to help support or control breathing. The autonomic nervous system (that regulates the functions of internal organs and some of the muscles in the body) can also be disturbed, causing changes in heart rate, blood pressure, toileting, or sweating. Therefore, the person should be put on a heart monitor or equipment that measures and tracks body function. Occasionally GBS-related nerve damage can lead to difficulty handling secretions in the mouth and throat. In addition to the person choking and/or drooling, secretions can fall into the airway and cause pneumonia.
Rehabilitative care
According to the NIS, as individuals begin to improve, they are usually transferred from the acute care hospital to a rehabilitation setting. Here, they can regain strength, receive physical rehabilitation and other therapy to resume activities of daily living, and prepare to return to their pre-illness life.
The NIH says complications in GBS can affect several parts of the body. Often, even before recovery begins, caregivers may use several methods to prevent or treat complications. For example, a therapist may be instructed to manually move and position the person’s limbs to help keep the muscles flexible and prevent muscle shortening. Injections of blood thinners can help prevent dangerous blood clots from forming in leg veins. Inflatable cuffs may also be placed around the legs to provide intermittent compression. All or any of these methods helps prevent blood stagnation and sludging (the buildup of red blood cells in veins, which could lead to reduced blood flow) in the leg veins. Muscle strength may not return uniformly; some muscles that get stronger faster may tend to take over a function that weaker muscles normally perform—called substitution. The therapist should select specific exercises to improve the strength of the weaker muscles so their original function can be regained.
Occupational and vocational therapy help individuals learn new ways to handle everyday functions that may be affected by the disease, as well as work demands and the need for assistive devices and other adaptive equipment and technology, the NIH says.
It is important to note, vaccines from Pfizer and Moderna are not affected by this warning.
The Associated Press and the National Institute of Health contributed to this article.